An idea inspired by the idea of a "magic bullet"
It was decades ago that scientists invented the concept of the so-called magic bullet, i.e. a drug that targets only diseased cells. Polish researchers have decided to put this idea into practice. They have created miniature "bubbles" – capsules approximately 100 nanometres in diameter (a million times smaller than a grain of sand) that can deliver the drug directly to cancer cells.
Drugs like paclitaxel (one of the most toxic, yet effective, chemotherapy drugs) have the disadvantage of being virtually insoluble in water, even though the human body is made up of 70% water. Microcapsules make it possible to "smuggle" them where they are needed – into cancer cells
– says dr hab. Szwed
How does it work?
Let us imagine a small ball whose "shell" is made of molecules of the well-known, water-soluble surfactant sodium dodecyl sulfate (SDS).
These molecules have two parts: hydrophilic heads that love water and hydrophobic tails that avoid water. Under the right conditions (stirring, presence of poly-L-lysine, appropriate temperature), the so-called micelles are formed, or spheres that encapsulate water-insoluble drugs, such as paclitaxel. Additionally, the entire structure is coated with a layer of poly-L-glutamic acid, which makes the capsules more "invisible" to the immune system. This allows them to circulate longer in the body and reach their target more effectively.
A cancerous tumour is not an orderly biological structure. It's chaotic, with large, irregular intercellular spaces. Thanks to their size and charge, capsules have a greater chance of becoming lodged in this disordered tumour environment and slowly releasing the drug there
– adds dr hab. Szwed
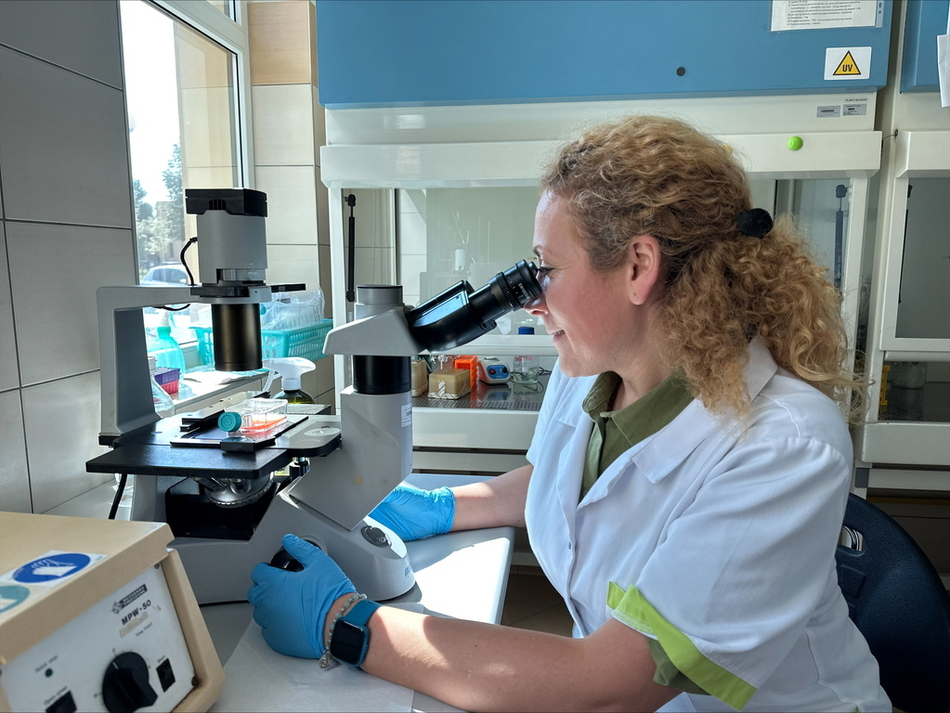
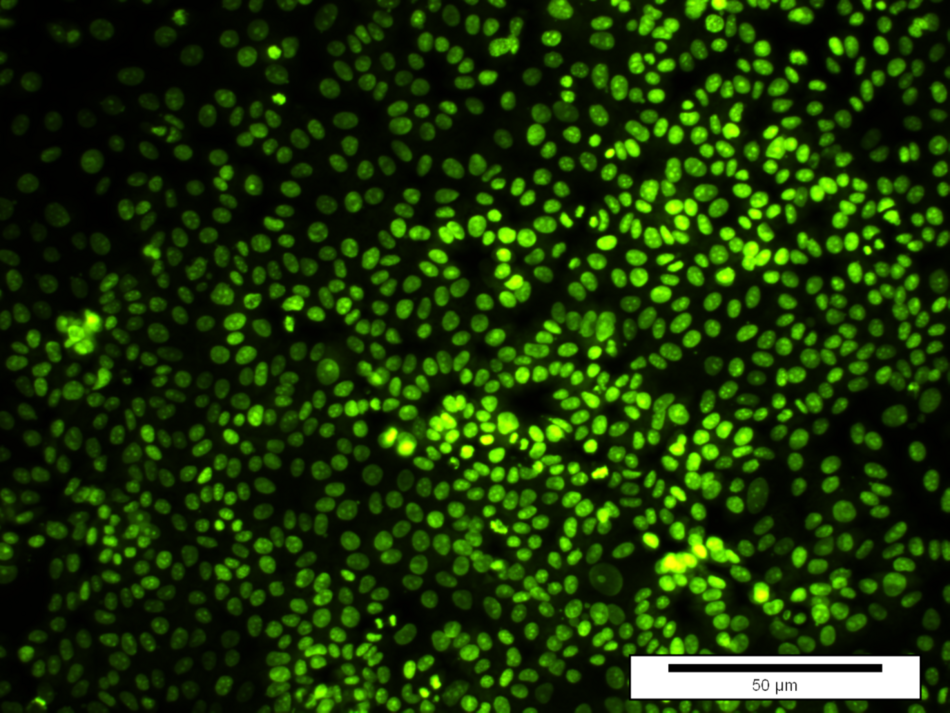
 Human breast cancer cells (MCF-7): control (untreated)
Human breast cancer cells (MCF-7): control (untreated)
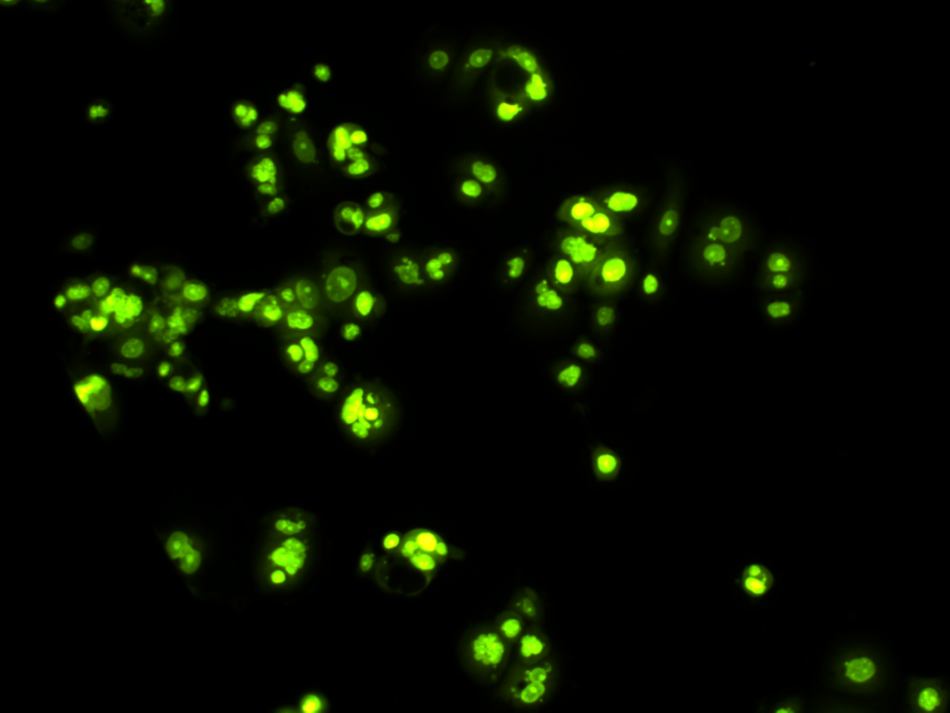
 Human breast cancer cells (MCF-7) 48 hours after adding the tested capsules (synthesised on the basis of SDS and filled with the anticancer drug – paclitaxel at a concentration of 10 nM) to the in vitro culture. After administration of the capsules, a clear decrease in the number of cells and a reduction in the rate of their division were noted. The cells were stained with the fluorescent marker CyQuant
Human breast cancer cells (MCF-7) 48 hours after adding the tested capsules (synthesised on the basis of SDS and filled with the anticancer drug – paclitaxel at a concentration of 10 nM) to the in vitro culture. After administration of the capsules, a clear decrease in the number of cells and a reduction in the rate of their division were noted. The cells were stained with the fluorescent marker CyQuant
The photos were taken during microscopic observations (Olympus IX70 fluorescence microscope, owned by the Department of Medical Biophysics, University of Lodz), magnification 10 x 10.
What do these capsules look like?
When we read about capsules, we often imagine transparent, oblong ampoules, like tablets that can be swallowed. However, these capsules are completely different. They don't have a hard shell and don't resemble the medications you're used to buying at pharmacies. They're so small they're invisible to the naked eye. The medication is still contained in a test tube, a clear liquid. The capsules are "hidden" within, floating in suspension like microscopic beads. Although invisible, they surround the most valuable substance – the anticancer drug, protecting it and directing it to where it's truly needed.
Can it be already used it in hospitals?
No, it can’t. The invention is currently at the basic research stage, which was made possible thanks to funding from the National Science Centre (NCN) for the MINIATURA 4 research project. This means that the tests were conducted in the laboratory, on cells grown in dishes, outside the human body. The next steps involve tests on cells in a 3D system (more resembling the conditions in the body), in vivo studies – i.e. on animals, and later, perhaps in cooperation with pharmaceutical companies, clinical trials on humans.
The path from invention to a drug in a pharmacy takes at least 12 years of work, but the results are already very promising
– says dr hab. Szwed
Invisible capsule – great hope
Although it's not yet available in pharmacies, this invention has the potential to transform the way we administer chemotherapy. Thanks to these intelligent capsules, we will be able to deliver the drug directly to cancer cells, sparing patients unnecessary suffering. This is another step toward medicine of the future – more targeted, effective and safe.
Source: dr hab. Marzena Szwed, Department of Medical Biophysics, Faculty of Biology and Environmental Protection, University of Lodz
Edit: Kacper Szczepaniak, Promotion Centre, Faculty of Biology and Environmental Protection, University of Lodz